Healthcare organizations are juggling patient needs, updating charts, and coordinating with colleagues. With so much happening, it's easy to see how mistakes can be made.
Unfortunately, even a minor, well-intentioned slip-up can have significant consequences if it involves patient privacy. These are the unintentional HIPAA violations that can keep practice managers and compliance officers up at night.
The Health Insurance Portability and Accountability Act (HIPAA) isn't just a set of arbitrary rules; it's a federal law designed to protect sensitive protected health information (PHI). While most healthcare professionals would never dream of deliberately exposing patient data, accidental HIPAA violations happen more often than you might think.
This article breaks down the problem and provides a solution-oriented framework. We'll explore common examples of unintentional HIPAA violations, outline the potential fallout, and provide actionable steps to take if an accidental breach occurs.
What is an accidental HIPAA violation?
An accidental HIPAA violation is the unauthorized disclosure, access, or use of Protected Health Information (PHI) that occurs without malicious intent. It's an "oops" moment that compromises patient privacy. PHI is any identifiable health information, including a patient's name, address, date of birth, Social Security number, medical records, or even the fact that they are a patient at your facility.
This framework applies to two main groups:
- A covered entity: This includes healthcare providers (hospitals, clinics, doctors), health plans (insurance companies), and healthcare clearinghouses.
- Business associates: These are third-party vendors that handle PHI on behalf of a covered entity. This could be a billing company, an IT provider, or a cloud storage provider. A covered entity is not only responsible for its own HIPAA compliance but also for the compliance of its vendors. This is managed through a formal Business Associate Agreement (BAA), which legally binds business associates to the same PHI protection standards.
The key difference between an accidental and a willful violation is intent. However, the Office for Civil Rights (OCR)-the enforcement arm of HIPAA-still takes these accidental disclosures very seriously, as they can cause significant harm to patients.
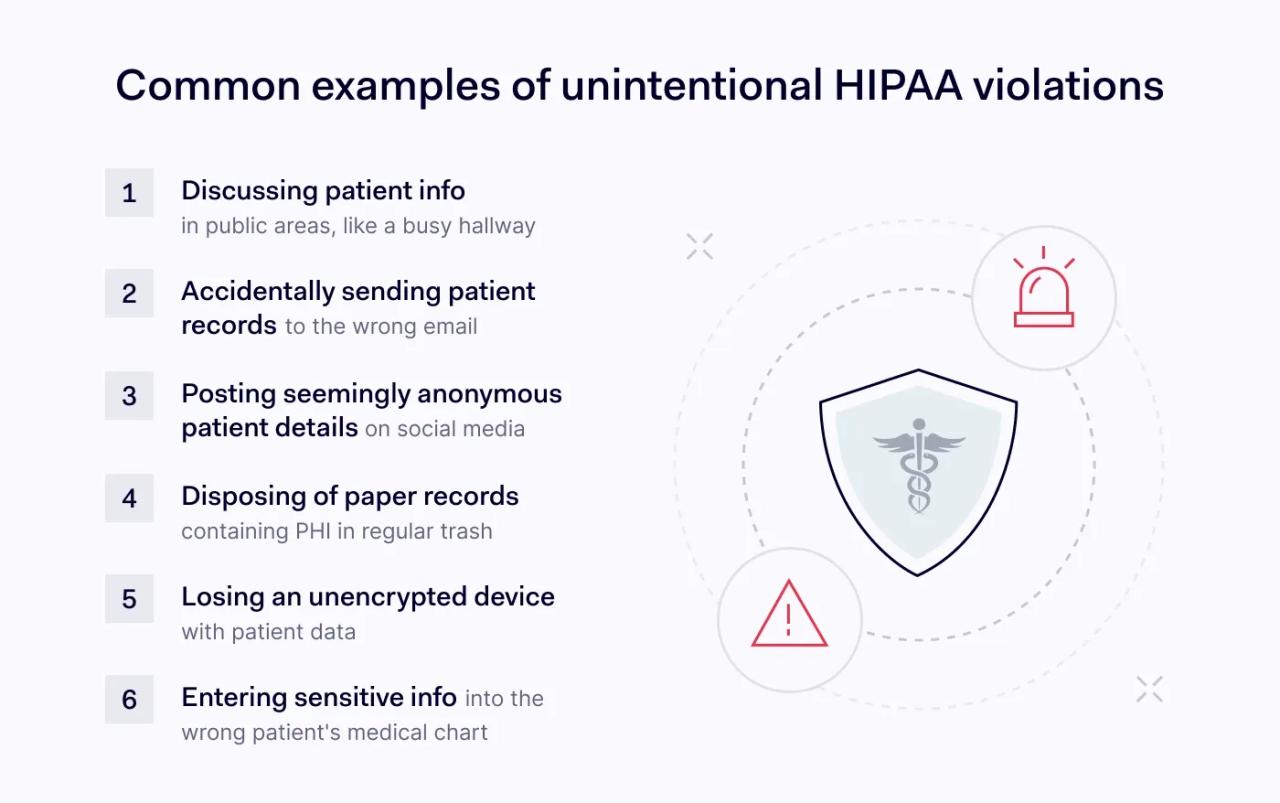
6 common examples of unintentional HIPAA violations
Many HIPAA violations stem not from malice but from simple human error, workflow gaps, or a lack of awareness. Here are some of the most common scenarios we see.
1. The "hallway consultation"
The problem: Two clinicians are discussing a complex patient case while walking down a busy hallway or riding in a public elevator. They might be trying to solve a problem efficiently, but they are inadvertently broadcasting PHI to anyone within earshot: other patients, visitors, or staff members who have no need to know.
Why it's a violation: Verbal disclosure of protected health information in a non-secure area is a classic example of an accidental breach. Even if names aren't used, enough detail can be shared to make a patient identifiable.
The solution:
- Establish private, secure areas for clinical discussions.
- If a quick conversation is necessary in a semi-public area, be mindful of volume and proximity to others.
- Always operate on a "minimum necessary" or "need-to-know" basis. Only discuss PHI with colleagues who are directly involved in that patient's care.
2. The misdirected email or fax
The problem: An administrative assistant is sending patient records to another provider for a referral. In a rush, they mistype a single digit in the fax number or a single letter in the email address. The sensitive documents, containing a patient's entire medical history, are now in the hands of a complete stranger.
Why it's a violation: This is a direct, unauthorized disclosure of PHI that can be classified as a data breach. Simple typos are one of the leading causes of accidental disclosures, and they can have massive consequences.
The solution:
- Double-check everything
- Use cover sheets: Always use a HIPAA-compliant fax cover sheet with a confidentiality notice.
- Use secure email portals that require recipient verification. For faxing, use systems that provide delivery confirmation and pre-program frequently used, verified numbers to reduce manual entry errors.
3. The social media slip-up
The problem: A nurse has a particularly heartwarming or challenging day at work. They post a vague story on their personal Facebook page about a "brave pediatric patient" they treated, including details about the case, but no name. A colleague comments, "Oh, I know who you mean! Room 302. So sad."
Why it's a violation: Even without a name, details can make a patient identifiable to their friends, family, or community members who may see the post. This is a severe violation of trust and privacy. The comment from the colleague confirms the identity, creating a definitive data breach. These types of accidental violations are particularly dangerous because they spread so quickly online.
The solution:
- A zero-tolerance social media policy: Your organization needs a crystal-clear policy stating that no patient-related information, no matter how anonymized it seems, should ever be posted on personal or professional social media accounts.
- Ongoing training: Regularly remind staff that their online activities can have real-world consequences for their job and the organization's HIPAA compliance. Explain that venting about work online is never a safe bet.
4. Improper disposal of PHI
The problem: At the end of a long day, a staff member is cleaning up their desk. They toss old appointment lists, sticky notes with patient names, and printed lab results into the regular office trash can. The trash is then placed in a dumpster outside, accessible to the public.
Why it's a violation: PHI in physical form must be rendered unreadable and indecipherable before it is disposed of. Tossing it in the regular trash leaves it vulnerable to "dumpster divers" and constitutes a serious compliance failure.
The solution:
- Place locked shred bins in all areas where PHI is handled. Make them as accessible as regular trash cans.
- The simplest and most effective approach is to implement a "shred-all" policy for any paper generated in patient care areas. This removes the guesswork for employees.
- Partner with a certified shredding service: Ensure your vendor is a business associate who provides a certificate of destruction. This professional relationship must be formalized with a business associate agreement.
5. Lost or stolen devices
The problem: A physician uses a personal, unencrypted laptop to review patient charts from home. They leave the laptop in their car overnight, and the car is broken into. The laptop, containing the PHI of hundreds of patients, is gone.
Why it's a violation: This is a catastrophic data breach that puts the covered entity at significant risk. The loss of an unencrypted device containing PHI is one of the most serious unintentional HIPAA violations. The organization has lost control of a massive amount of patient data, triggering significant breach notification requirements.
The solution:
- Encryption: Encrypt devices that store, access, or transmit ePHI consistent with the Security Rule's addressable encryption requirements. When properly implemented, encryption can provide breach-notification safe harbor.
- Strong device security policies: Enforce strong passwords, two-factor authentication, and automatic screen locks.
- Prohibit use of personal devices: Where possible, issue company-owned, secured devices. If a BYOD (Bring Your Own Device) policy is necessary, it must be strictly managed with mobile device management (MDM) software.
6. The "wrong chart" error
The problem: In a busy emergency room, a nurse is documenting vitals and accidentally opens the chart of John Smith, born in 1975, instead of John Smith, born in 1985. They enter sensitive information into the wrong patient's record. Alternatively, a front-desk employee hands a patient discharge papers that belong to someone else.
Why it's a violation: This results in two HIPAA violations: the integrity of the patient data in the wrong chart is corrupted, and the patient who receives the wrong paperwork has been given unauthorized access to another person's PHI.
The solution:
- Active patient identification: Before accessing or providing any PHI, use at least two patient identifiers (for example, full name and date of birth).
- EHR safeguards: Modern Electronic Health Record (EHR) systems often include photo identification and pop-up alerts to help prevent this type of error. Ensure these features are enabled and staff are trained to use them.
The aftermath of accidental HIPAA violations
When an accidental violation occurs, the consequences can be severe, even if there was no malicious intent. The Office for Civil Rights investigates complaints and can impose significant financial penalties based on the level of negligence involved. The role of the Office for Civil Rights (OCR) is to enforce HIPAA rules, and they take all reported breaches seriously.
The penalty structure is tiered:
- Tier 1 (Lack of knowledge): penalties range from $141 to $71,162 per violation (annual cap $2,134,831), adjusted annually.
- Tier 2 (Reasonable cause): The covered entity had reasonable cause to believe it was compliant but not acting with willful neglect. Penalties range from $1,424 to $71,162 per violation (annual cap $2,134,831), adjusted annually.
- Tier 3 (Willful neglect, corrected): The violation resulted from willful neglect, but the entity corrected the issue within 30 days. Penalties range from $14,232 to $71,162 per violation (annual cap $2,134,831), adjusted annually.
- Tier 4 (Willful neglect, not corrected): The entity demonstrated willful neglect and made no effort to correct the violation. Penalties range from $71,162 to $2,134,831 per violation (annual cap $2,134,831), adjusted annually.
Beyond financial penalties, a breach can lead to mandatory corrective action plans, reputational damage, loss of patient trust, and potential termination for the individuals involved.
A step-by-step guide: responding to an accidental breach
Discovering one of these accidental violations can be panic-inducing, but a calm, systematic response is crucial. Hiding the mistake is the worst thing you can do.
- Immediate action & reporting: The moment a potential breach is discovered, the individual must stop what they are doing and immediately report it to their supervisor and the organization's designated Privacy Officer.
- Contain the breach: Take immediate steps to mitigate the damage. This could mean recalling an email, retrieving improperly discarded documents, or remotely wiping a lost device.
- Conduct a timely risk assessment: The Privacy Officer must lead a formal risk assessment to determine the nature and extent of the breach. The HIPAA Breach Notification Rule requires this specific type of risk assessment to evaluate the probability that PHI has been compromised. It must consider:
- The nature and extent of the PHI involved.
- The unauthorized person who used the PHI or to whom the disclosure was made.
- Whether the PHI was actually acquired or viewed.
- The extent to which the risk to the PHI has been mitigated.
- Execute breach notification: Based on the results of the risk assessment, the organization must provide notifications.
- To affected individuals: All affected patients must be notified without unreasonable delay, and no later than 60 days after the discovery of the breach.
- To the Department of Health and Human Services (HHS): Breaches affecting 500 or more individuals must be reported to the OCR, and individuals must be notified at the same time. Smaller breaches are logged and reported to the OCR annually.
- To the media: If a breach affects more than 500 residents of a single state, prominent media outlets in that state must also be notified.
Conclusion: prevention is the best medicine
While knowing how to respond to accidental HIPAA violations is critical, the ultimate goal is prevention. The examples of unintentional HIPAA violations discussed here are not rare; they are everyday risks in any healthcare setting. Building a strong culture of HIPAA compliance is the most effective defense.
This requires more than a once-a-year training session. It demands robust policies, ongoing education, clear and accessible procedures, and the right technological safeguards. From encryption and secure email to a formal risk assessment framework, having the proper tools in place can turn a potential disaster into a managed incident.
To fortify your organization against these common but costly mistakes, consider partnering with compliance experts. A dedicated compliance platform can streamline everything from policy management and employee training to conducting a formal risk assessment and managing the aftermath of an accidental breach.
Investing in a proactive compliance strategy is not just about avoiding fines; it's about protecting your patients, your reputation, and the integrity of your practice as a covered entity and a trusted partner to your business associates.
Disclaimer: This article is for informational purposes only and does not constitute legal advice. The laws, regulations, and penalties discussed are subject to change and may have been updated since the time of publication. We recommend consulting with a qualified legal professional for guidance on your specific compliance needs.